
The Boston Diabetes Cardiology team believes that patients and families should be able to access quality healthcare at comfortable and most trusted centers when making their healthcare decisions.
Our highly-qualified team of Cardiologists and support specialists provide patients with the latest advance care for disorders of the heart. We offer a wide range of cardiac care services and treatments and a full array of diagnostic tests that are quality driven, comprehensive, patient-centered cardiovascular care.
The individual treatment programs and a regular follow up are provided by the specialists
The following are the core services provided by the department personnel:
Exercise electrocardiography or Stress tests (TMT)
24 Hour Holter Monitoring
Echocardiography with Color Doppler Study
ECG
Ambulatory Blood Pressure monitor
The recording of the heart's electrical activity and blood pressure while the heart is under the physical stress. This is also known as an exercise tolerance test.
A cardiac stress test is used to assess the heart muscle's response to the need for additional oxygen, which occurs during increased physical activity. This procedure is most often done for the following reasons:
Prior to Procedure your doctor will likely do a physical examination and will review your medications as some should not be taken before testing. Resting electrocardiogram (ECG) and Echocardiogram might be done too.
Instructions before undergoing the procedure:
No anesthesia required in this procedure.
During all types of stress testing, a doctor, nurse, or technician will always be with you to closely check your health status. Before you start the test, the nurse will put sticky patches called electrodes on the skin of your chest, arms, and legs. To help an electrode stick to the skin, the nurse may have to shave a patch of hair where the electrode will be attached.
The electrodes will be connected to an electrocardiogram machine. This machine records your heart's electrical activity. It shows how fast your heart is beating and the heart's rhythm (steady or irregular).
The nurse will put a blood pressure cuff on your arm to check your blood pressure during the stress test. (The cuff will feel tight on your arm when it expands every few minutes.) Also, you might have to breathe into a special tube so the gases you breathe out can be measured.
Next, you'll exercise on a treadmill or stationary bike. If such exercise poses a problem for you, you might turn a crank with your arms instead. During the test, the exercise level will get harder. You can stop whenever you feel the exercise is too much for you.
If you can't exercise, medicine might be injected into a vein in your arm or hand. The medicine will increase blood flow through your coronary arteries and make your heart beat fast, as it would during exercise. You can then have the stress test.
The medicine may make you flushed and anxious, but the effects go away as soon as the test is over. The medicine also may give you a headache.
While you're exercising or getting medicine to make your heart work harder, the nurse will ask you how you're feeling. You should tell her if you feel chest pain, short of breath, or dizzy.
The exercise or medicine infusion will continue until you reach a target heart rate, or until you:
The nurse will continue to check your heart functions and blood pressure after the test until they return to normal levels.
The "stress" part of a stress test (when your heart is working hard) usually lasts about 15 minutes or less.
However, there's prep time before the test and monitoring time afterward. Both extend the total test time to about an hour for a standard stress test.


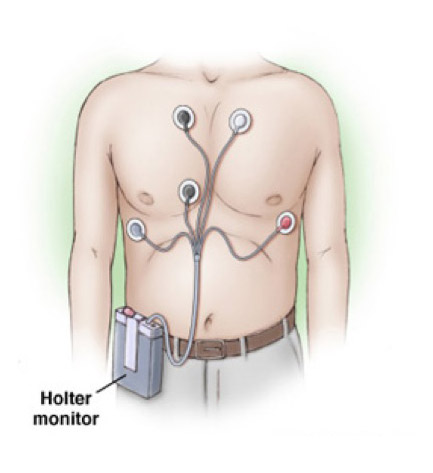
A Holter monitor is a battery-operated portable device that measures and tape records your heart’s activity (ECG) continuously for 24 to 48 hours or longer depending on the monitor used. The device is the size of a small camera. It has wires with silver dollar-sized electrodes that attach to your skin.
The heart is equipped with its own "wiring." It has specialized cells that conduct nerve impulses to keep the heart beating regularly at just the right rate. The heart can speed up or slow down in response to the body's need for oxygenated blood. Coronary artery disease or structural problems with the heart muscle, along with other conditions, can cause problems with the heart's conduction system.
You may feel a conduction problem as heart palpitations or a fluttering in your chest. The clinical term for this is "arrhythmia". This means the heart beats too quickly, too slowly or with an irregular pattern. Sometimes you will not have any symptoms that this is occurring. A Holter monitor checks the heart's electrical activity over several hours. It can also evaluate if an artificial pacemaker is working properly.
Holter monitoring is a continuous monitoring of heart rate and rhythm during your usual daily activities, usually for a 24-hour period. It is also called continuous ambulatory electrocardiographic monitoring.
Indication: Your Doctor may request this test
A Holter monitor is a noninvasive test. It is painless. The Nurse will attach the Holter monitor and instruct you how to record your symptoms while wearing it. The Nurse first attaches the electrodes to your chest. If you have a hairy chest, he or she may shave some hair off to attach the electrodes firmly. Once the electrodes are in place, the nurse helps you put the Holter monitor on and explains how to take care of it for 24 hours. You can carry the monitor in a pocket or pouch, slung across your shoulders and neck like a purse or camera, or attach it to your waist.
During the test, you may be asked to change positions or hold your breath for a short time. This allows the Doctor to get better pictures of your heart.
Do your usual activities while you wear the monitor with these exceptions :
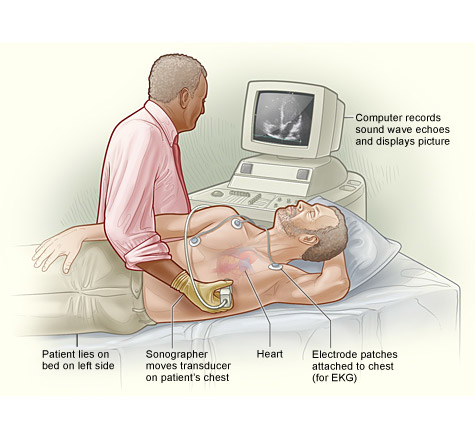
Echocardiography is a painless test that uses sound waves to create moving pictures of your heart. The pictures show the size and shape of your heart. It will also show how well your heart's chambers and valves are working. Echo also can pinpoint areas of heart muscle that aren't contracting well because of poor blood flow or injury from a previous heart attack. It can detect possible blood clots inside the heart, fluid buildup in the pericardium (the sac around the heart), and problems with the aorta (the main artery that carries oxygen-rich blood from your heart to your body).
Your doctor may recommend echocardiography
You will be asked remove your clothing from the waist up. Women will be given a gown to wear during the test. You'll lie on your back or left side on an exam table or stretcher. A doctor will apply gel to your chest. The gel helps the sound waves reach your heart. A device called a transducer will then be moved around on your chest. The transducer transmits ultrasound waves into your chest. A computer will convert echoes from the sound waves into pictures of your heart on a screen. During the test, the lights in the room will be dimmed so the computer screen is easier to see. The Doctor will record pictures of various parts of your heart.
During the test, you may be asked to change positions or hold your breath for a short time. This allows the Doctor to get better pictures of your heart.
At times, the Doctor may apply a bit of pressure to your chest with the transducer. You may find this pressure a little uncomfortable, but it helps get the best picture of your heart. You should let the sonographer know if you feel too uncomfortable.
For appointments please call 971 4 3805555.